Appendix 3: How HIV tests work
What is an antigen?
An antigen is a substance found on a foreign organism such as a virus or bacteria which, when it gets into the body, stimulates an immune response.
What is an antibody?
An antibody is a certain type of immune cell. In adults it is initially made when your body first recognises an antigen.
Antibodies are ‘Y’ shaped and the two arms of the ‘Y’ are known as the variable region. This means it is specifically coded to interact with a certain antigen, just as a key is specific for a lock (see Figure 14).
The stick of the ‘Y’ is the same in all antibodies (the constant region). It is the variable region (the two arms) that interract with and attach to the antigen.
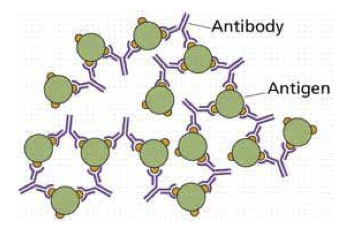
When the antibody sticks to the antigen it neutralises it so that the foreign organism can no longer enter a human cell or cause harm (see Figure 15).
Once an infectious agent is neutralised it dies.
Figure 14: Diagram of a Y-shaped antibody
The variable region – the antigen binding site (in yellow) and the constant region (in light blue)
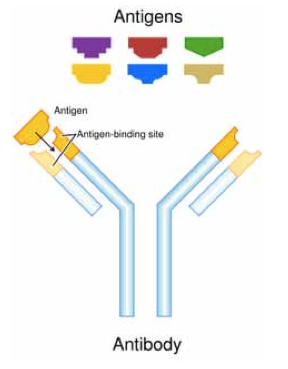
Figure 15: How antibodies and antigens interact
Antibodies neutralising an infectious particle.
How do antibodies and antigens interact?
One way to explain how an antigen and antibody interact is to compare them to a lock and key. The antigen acts like a lock and the antibody like a key. Each key is different for each lock.
As we grow, especially in childhood, we develop a library of millions of different antibodies. This makes up our acquired immune system.
This is a huge reference bank of immune cells that are generally resting or sleeping until they are needed.
Most HIV tests are based around this interaction. On the surface of HIV there are lots of proteins which act as antigens. One of the most common in early infection is called protein 24 (p24).
Antigens for HIV are detectable in most people around 16 days after infection.
Antibodies take longer to produce and are not usually detectable until 4-12 weeks after infection.
How does an ELISA test detect HIV antibodies?
ELISA tests are the standard test for finding out if someone has antibodies to a particular antigen. ELISA stands for enzyme-linked immunosorbent assay.
It is performed in 4 steps as shown in Figure 15.
Rapid tests
Rapid tests are a simplified version of antibody ELISA tests. They look for HIV antibodies in the blood. The antigens for HIV are fixed on one particular strip along the rapid test stick. Towards the end of the testing stick are control antigens to show that the test worked.
A sample is placed at the end of the testing stick. A chemical, called a buffer, to facilitate the testing process is added.
The chemical causes the antibodies in the blood to flow along the test stick. When they pass over the section with the antigens, if there are any antibodies for HIV present then they will stick to these antigens and change colour.
Once the test is complete, if there is one stripe it means it is a negative result. If there are two stripes then it means it’s a positive result. If there are no stripes it means the test did not work properly.
This is illustrated in Figure 10 earlier in this guide.
Figure 16: ELISA antibody detection test
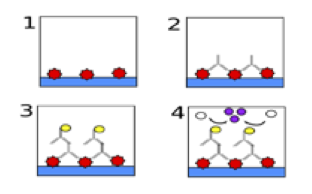
- HIV p24 antigens are manufactured and attached to the bottom of a plastic testing dish.
- The dish is then washed with the blood sample. If antibodies (upside-down Y-shapes) for the p24 antigen are present then they attach to the antigens in the dish. This gives an HIV positive result. If antibodies are present the steps 3 and 4 follow. If there are no antibodies, only antigen remains and this is a negative result.
- Once the antibodies are attached to the p24 antigen, they need to be made visible. To do this the dish is washed with a second ‘marker’ antibody. The second antibody is specific to all human antibodies. When it comes into contact with a human antibody it will attach itself. This second antibody has an invisible ‘marker’ attached to the end of it (represented by the black circle)
- Finally the dish is washed with a dye. Where the second ‘marker’ antibody is present, the marker (represented by the light circle) will cause the liquid in the dish to change colour (represented by the dark circles). Where there is no ‘marker’ antibody the liquid will remain clear. This means that any dish that is coloured is a positive result and any dish containing clear liquid is a negative result.
How does an ELISA test detect p24 antigen?
An ELISA to detect antigens is called a sandwich ELISA and works in a similar way (see Figure 17).
Figure 17: ELISA antigen detection test
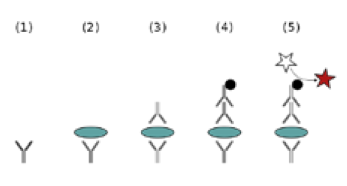
- Antibodies for p24 (represented by the Y-shaped picture below the number (1)) are secured to the bottom of a Petri dish.
- The blood sample is added to the dish and if the sample is HIV positive then the p24 antigen on the surface of HIV (represented by the disc) will attach to the antibodies. If the blood sample is negative then there will be no antigens and the dish remains the same as in number (1)
- An antibody specific to the p24 antigen is then added to the dish and where the p24 antigen is present it attaches. If there is no p24 antigen present then it washes away
- Once the antibodies are attached to the p24 antigen, they need to be made visible. To do the dish is washed with a second ‘marker’ antibody. The second antibody is specific to all human antibodies. When it comes into contact with a human antibody it will attach itself. This second antibody has an invisible ‘marker’ attached to the end of it (the small dark circle)
- Finally the dish is washed with a dye. Where the second ‘marker’ antibody is present, the marker (represented by the black circle) will cause the liquid in the dish to change colour (represented by the stars). Where there is no ‘marker’ antibody the liquid will remain clear. This means that any dish that is coloured is a positive result and any dish containing clear liquid is a negative result.
Third generation tests are an ELISA that looks for an antibody alone. Fourth generation tests use both of the above methods to look for both antibodies and antigens.
What does the number after the HIV ELISA test result mean?
Some people are given test results which say something like ‘non-reactive (OD: 0.219)’. This number at the end is called the Optical Density (OD) value. This is the measure of how much colour there is in the dish at the end of the ELISA.
As the colour in the dish is an indicator of whether the result is negative or positive these numbers give the result more precisely than just a simple ‘positive’ or ‘negative’ answer.
The cut-off values for different tests vary. In general, any numbers below 1.0 mean it’s a negative result. Any numbers above 1.0 mean it’s a positive result.
The numerical results of HIV tests are not related so if someone has 2 tests and the numbers look like they are increasing it does not mean they are slowly becoming positive. It is just two separate figures.
If someone has an ‘inconclusive’ test result it is possible that the OD is very close to 1.0 and a confirmatory test will have to be done.
How does a western blot test work?
The western blot, is similar to the ELISA in that it also detects antibodies for HIV. However, it works slightly differently to an ELISA. A western blot works by detecting antibodies to lots of specific proteins (antigens) at the same time.
To do the test, HIV is split into its various component proteins which are all different lengths and thus different weights (measured in kD – kilo Daltons). A blood sample is then mixed with the proteins and any antibodies for HIV in the blood sample attach to the proteins in a similar way to that in the ELISA outlined above. The antibodies present are then tagged using ‘marker’ antibodies (see ELISA section).
Each sample is then added to a dip made in a special gel. The gel is then plugged into an electric current and the proteins start to move down the gel.
The heavier proteins stop quicker than the lighter ones. The more there are of each protein, the thicker and darker the stripes. The gel is then developed in a similar way to a non-digital photograph to show which proteins are present.
If there are stripes where the HIV proteins should be then the result is positive. If there are no stripes then the result is negative.
The difference between the western blot and the ELISA is that the western blot can identify antibodies for lots of different HIV proteins or antigens at the same time whereas the ELISA will only look for one at a time (see Figure 18 and 19).
Figure 18: A drawing of results of a western blot test
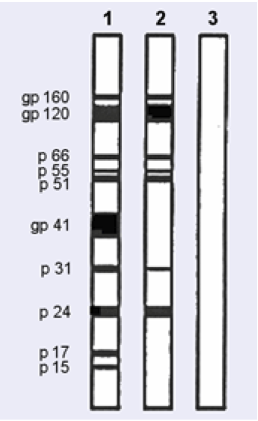
In this case Test 1 is a control as it shows all the proteins tested for are present.
Controls are crucial to make sure that the test is working correctly.
Test 2 is a positive result as it shows there are antibodies for 7 of the HIV proteins.
Test 3 is a negative result.
Figure 19: Western blot test result
In reality a western blot does not look as neat as Figure 18 but looks more like the stripes below.
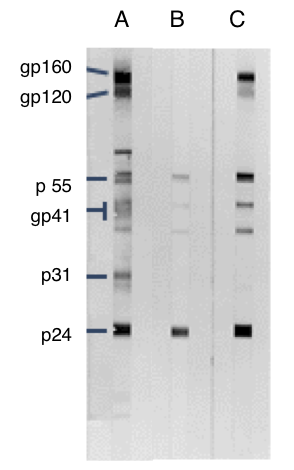
A – control strip showing antibody responses to key HIV proteins
B – Indeterminate response showing antibodies to p24
C – Positive western blot showing responses to at least three key proteins
PCR tests: DNA and RNA (viral load)
The polymerase chain reaction (PCR) test looks for genetic material from the HIV virus itself.
This genetic material can be RNA (single strand) or DNA (double strand).
RNA and DNA are long chains of chemicals. Different sections of this genetic material are like recipe books for making new virus.
A sample is amplified many times so that there is enough RNA or DNA to be measured.
DNA tests are used for testing babies born to HIV positive mothers and results are positive or negative.
RNA is used for viral load tests for most adult testing, including monitoring HIV positive people before and after treatment.
The PCR test produces a quantifiable result, which means that, as well as a negative/positive result, the amount of virus present in the sample can also be detected.
This result is given as copies per millilitre (copies/mL). The sensitivity of the test is usually 50 copies/mL, below which a result is referred to as undetectable.
How is the accuracy of HIV tests measured?
Accuracy of medical tests are often described in terms of:
Sensitivity – the percentage of the results that will be positive when HIV is present
Specificity – the percentage of the results that will be negative when HIV is not present.
The ideal test would have 100% sensitivity and 100% specificity, but few tests are ever this accurate.
Every diagnostic test has its limitations. On very rare occasions the results can be inconclusive or incorrect.
These are either false positive – the test result indicates that HIV is present when it is not or false negative – the test result indicates that HIV is absent in an infected person.
A second confirmatory test would eliminate this possibility. False negative and false positive results are discussed in the section ‘Test accuracy, results and further testing‘.
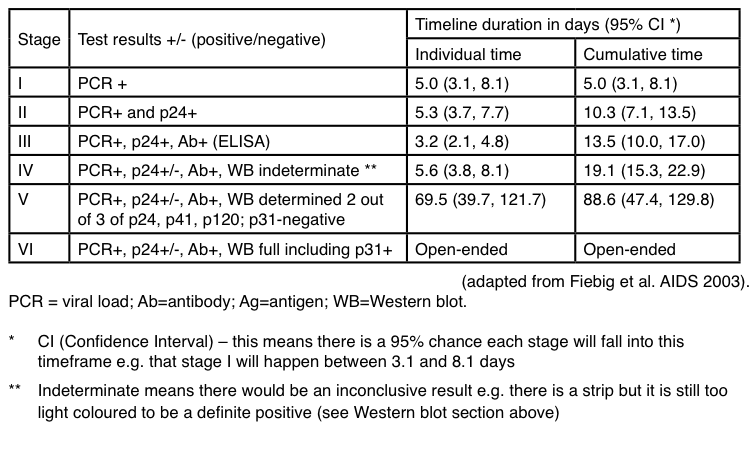
Stages of seroconversion
Stages of seroconversion and primary HIV infection by looking at the time that different HIV tests gave a positive reaction are shown in Figure 20.
Every one has their own immune system and response to infections. This table shows how difficult it is to say exactly when each test is accurate as there is such individual variation.
To help visualise the timeframe for the number of days after infection that each laboratory stage can pick up primary infection see Figure 11 earlier in this guide.
Figure 20: Stages of seroconversion when different laboratory tests can detect HIV
Last updated: 1 June 2021.
