Low- and middle-income countries defuse hepatitis C
30 June 2013. Related: Pipeline report, Hepatitis coinfection, Virology.
By Karyn Kaplan
As rich countries prepare for a hepatitis C virus (HCV) treatment revolution, people in low- and middle-income countries (LMICs) remain without access to information, prevention tools, diagnostics, care, and treatment. A growing movement of global activists is responding to this crisis.
They are demanding access to affordable, quality drugs and diagnostics as well as high-level political commitment to testing and treatment scale-up in their countries. They will continue to fight until they defuse what the World Health Organization (WHO) has called the “viral time bomb.”
An estimated 185 million people (three percent of the world’s population) are infected with hepatitis C virus (HCV). Globally, the majority of new HCV infections are occurring among the estimated 15.9 million people who inject drugs (PWID); at least 10 million of them have HCV. Yet less than 10 percent of the world’s PWID have access to harm reduction services such as needle and syringe programs and opioid substitution therapy (OST), promoting further HCV transmission. [1, 2]
Untreated hepatitis C can lead to cirrhosis, liver failure, and liver cancer; each year, more than 350,000 people die from these complications. [3] Despite widespread prevalence and increasing morbidity and mortality, the global response to the HCV epidemic has been sluggish.
HCV finally gained recognition as a global public health priority in 2010, when the World Health Assembly (WHA; the decision-making body of the WHO) called for comprehensive programs that “enhance access to affordable treatment in developing countries.” [4]
Since then, excitement around new, more effective HCV treatment—and outrage that little has been done to address the epidemic—has motivated a diverse coalition of stakeholders: people living with and at risk for HCV and HIV; people who use illicit drugs; researchers; health care and harm reduction providers; nongovernmental organizations (NGOs); and others, including progressive government leaders. A global movement for HCV treatment access has begun.
From Ukraine to India, and from Georgia to Egypt, activists from LMICs are adapting relevant lessons from the HIV treatment-access movement about how to reduce the cost of drugs and diagnostics, integrate services, and simplify the package of care. They are demanding that their governments take action to address local epidemics and include civil-society representatives meaningfully in the response.
We’ve Got to Get It Together, Because the Revolution Is Here
In LMICs, people living with hepatitis C and their allies are excited about the simpler, better treatments on the horizon, but they wonder what this treatment “revolution” will mean for them. Significant barriers, ranging from widespread lack of awareness about HCV to the high cost of diagnostics and medication, must be overcome in order to achieve widespread access to these safer, more effective treatments as well as to the current standard of care.
Strategies for addressing the HCV epidemic and increasing access to treatment include:
- the repeal of repressive laws that criminalize people who use drugs;
- massively increasing access to evidence-based harm reduction services including clean injecting equipment and OST;
- ensuring access to safe, effective, and affordable HCV treatment with or without pegylated interferon (peginterferon or PEG-IFN); and
- identifying and prioritizing people with urgent need for treatment.
Some Governments Have Begun the Revolution
Egypt
One government stands out for its successful commitment to stopping HCV: Egypt. With six million people (10 percent of its population) who have chronic HCV, Egypt is home to the world’s largest HCV epidemic. [5] Unsafe injections inadvertently given during a mass anti-schistosomiasis campaign spread HCV across the country. Schistosomiasis (caused by parasitic diseases) was the leading cause of liver disease before being eclipsed by HCV. [6] Unfortunately, HCV coinfection accelerates liver disease in people with this illness. [7]
In response to the HCV epidemic, the Egyptian government developed the world’s largest nationally subsidized viral hepatitis–control program. Egypt’s Ministry of Health and Population established a National Committee for the Control of Viral Hepatitis, which in turn developed a National Control Strategy for Viral Hepatitis. Egypt’s initiatives include:
- conducting a national prevalence survey and ongoing surveillance;
- launching awareness campaigns and prevention programs;
- establishing clinical research programs, including programs to evaluate their work;
- developing national HCV treatment guidelines; and
- opening dozens of treatment centers to augment existing health care sites.
Egypt continues to enhance and develop its national program, which may serve as a model for other LMICs.
More than 220,000 people have already been treated for hepatitis C under Egypt’s program. The government continues to negotiate lower drug prices to facilitate provision of treatment to everyone who needs it.
Lowering the cost of PEG-IFN has made it possible for Egypt to tackle its epidemic. A locally produced product (Minapharm’s Reiferon Retard), a competing version of peginterferon, provided leverage for negotiations with Roche and Merck, the makers of Pegasys (PEG-IFN alfa-2a) and Peg-Intron (PEG-IFN alfa-2b), respectively. Over the past six years, the Egyptian government has obtained a sixfold price reduction, from US$12,000 to US$2,000 per 48-week treatment course. [8]
Thailand
In Thailand, 2.2 percent of the population (1.4 million people) has HCV. Prevalence among PWID in Thailand is estimated to be over 90 percent. [9]
Over the past several years, civil-society groups have pressured the government to address Thailand’s unchecked HCV epidemic, demanding that PEG-IFN be added to the National Essential Medicines List (EML). Through community organizing and education, policymaker lobbying meetings, and direct actions, Thai AIDS Treatment Action Group (TTAG), the Thai Network of People Living with HIV/AIDS (TNP+), and others, secured a government commitment to expand HCV treatment access through the national healthcare scheme. In August 2012, Thailand put PEG-IFN on its national EML.
The government, propelled by grassroots activists, successfully negotiated a significant (fourfold) price reduction from Roche and Merck: US$4,800 per treatment course. Because of powerful civil-society advocacy and government negotiations with pharmaceutical companies, Thailand was able to afford including HCV treatment in its universal health care program. But activists realize the price of drugs and diagnostics must come down further to make widespread access possible—and they continue to pressure their government.
India
At least 1.5 percent of India’s population (nearly 2 million of more than 1 billion people) has hepatitis C, including most people who inject drugs. [10] India, whose generic drug industry is known as the “pharmacy to the developing world,” recently issued two court rulings that defied efforts by two multinational drug companies to make claims on patents for old drugs they alleged to be new, including PEG-IFN. These rulings pave the way for people in India (and other places where these drugs are not patented) to gain access to more affordable medications by facilitating production of biosimilars. [11]
Biosimilars
Biologic drugs—such as peginterferon, insulin, and monoclonal antibodies—are made in living cells. In contrast, generic medications are made with the same active ingredients used in the innovator (branded) product. Generic drugs must demonstrate therapeutic equivalence to the original: they must be “the same chemically as their innovator counterparts and…act the same way in the body.” [12] Generic biologics, which must demonstrate similarity (but cannot demonstrate equivalence) and show that they work as well as the branded product, are called “biosimilars.” In addition, there are “alternative” types of PEG-IFN, which, unlike biosimilars, do not need to demonstrate similarity. Neither is identical to the innovator product; therefore, the regulatory pathway for determining the quality, safety, and efficacy of biosimilars and alternatives, which cannot be compared with original products, is less clear.
In 2012, Sankalp Rehabilitation Trust, a local NGO working with PWID, brought a court challenge to Roche’s patent on peginterferon alfa-2a. The Intellectual Property Appellate Board (IPAB) ruled in favor of Sankalp as a “person interested,” and therefore able to legitimately bring the case to court. The IPAB then overturned Roche’s patent—Sankalp had successfully challenged its validity. The IPAB found that Roche’s product was not innovative, and was therefore unworthy of a patent. It ruled that Sankalp’s effort could help “break the monopoly” on PEG-IFN and “bring the drug within reach of the community for whom it works, not only by reduction in cost, but also because of increase in supply.” [13]
An activist campaign launched by Lawyers Collective and grassroots networks including the Indian Network of People Living with HIV/AIDS (INP+) and the Delhi Network of Positive People (DNP+) made these court cases possible. In April 2013, India’s Supreme Court struck down an appeal by pharmaceutical giant Novartis. The court ruled that its anticancer drug, a beta-crystalline form of imatinib (known as Gleevec, or Glivec), was not patentable because it was too similar to an earlier version of the medicine, and no more effective. [14] In India, an alternative imatinib is available for US$2,500 for a year’s course; in the United States, the branded product costs US$70,000. [15] As with PEG-IFN, people in India and others in countries where imatinib is not patented can now continue to access more affordable biosimilars.
These court-based wins bring affordable drugs—including hepatitis C treatment—closer to billions of people in the world, rather than keeping essential medications priced cruelly out of reach.
Ukraine
In April of 2013, activists in Ukraine who called themselves “the Condemned,” wore cloth hoods over their faces and protested in front of the offices of the Cabinet of Ministers, the country’s highest executive political body. They demanded that the ministers immediately implement a presidential order to allocate funding for the treatment of life-threatening diseases, including HCV, which they estimate will kill at least 44,000 people in Ukraine this year. [16] Within weeks, the government agreed to develop a funded national plan.
Georgia
In Georgia, 6.7% of the population (or at least 200,000 people) has HCV, yet less than one percent has access to treatment. Civil-society advocates in Georgia, including the Georgian Harm Reduction Network (GHRN), have been pushing their government for a fully funded national program. Activists are making progress through lobbying parliamentarians and meeting with ministers.
This year, Georgia’s Ministry of Corrections committed to treat 300 people in prison who have HCV, expanding to 500 in the next year. Activists are pushing the government to encourage the Ministry of Labor, Health and Social Affairs (MoLHSA) to also treat people with HCV.
Global Strategies for Access
Most people with hepatitis C live in LMICs, where the cost of treatment can exceed per-capita Gross Domestic Product (GDP) tenfold. [17] (See figure 1. Cost of a 48-Week Course of Brand-Name PEG-IFN Treatment vs. Gross Domestic Product (GDP) per Capita.) Activists are promoting a range of successful advocacy strategies, including price negotiations with pharmaceutical companies, the use of compulsory licenses, and promoting the use of quality, affordable biosimilars to push for access where even the standard of care is priced out of reach.
Figure 1. Cost of a 48-Week Course of Brand-Name PEG-IFN Treatment vs. Gross Domestic Product (GDP) per Capita
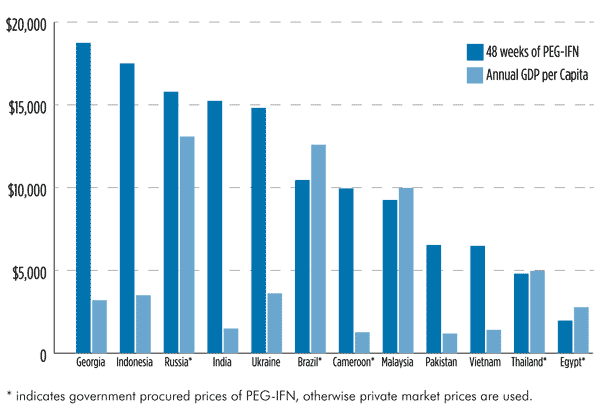
Sources:
- Cost of PEG-IFN from Momenghalibaf A. Global snapshot: HCV epidemiology and response (Draft). Open Society Foundations Access to Essential Medicines Initiative and International Harm Reduction Development Program. Forthcoming 2013.
- GDP per capita data from
http://data.worldbank.org/indicator/NY.GDP.PCAP.CD. (Accessed 2013 May 31)
Price Negotiations
Roche and Merck must drastically cut the price of PEG-IFN for LMICs. New HCV drugs must also be affordable. In the United States, a single course of HCV treatment with peginterferon, ribavirin, and telaprevir (an HCV protease inhibitor)—including managing side effects and posttreatment follow-up—costs US$98,348. [18]
On Valentine’s Day (February 14), 2013, international advocates joined Médecins du Monde and Treatment Action Group in launching an online social media campaign targeting Roche and Merck. The Valentine’s Day card, sent via e-mail, Facebook, and Twitter to company executives, read, “Have a heart, save my liver!” More than 30,000 valentines were sent during this one-day action. The slogan was accompanied by an incisive message about the need to slash drug prices to avert more than 350,000 annual HCV-related deaths.
Essential Medicines List
In 2012, Médecins Sans Frontières (MSF) submitted an application for PEG-IFN to be included on the World Health Organization’s Essential Medicines List (EML). [19] Once a drug is on the WHO EML, it is easier to get access to quality, affordable versions, as the EML guides procurement and supply as well as essential drug choices. Adding PEG-IFN to the EML sends a strong message to countries: treating HCV is a priority, and PEG-IFN is safe, effective, and cost-effective. [20] It encourages countries to prioritize inclusion of PEG-IFN on their national EMLs, thereby increasing its accessibility.
Compulsory Licenses
Some countries, including Brazil, Indonesia, Thailand, Ghana, and Cameroon, have issued compulsory licenses to increase access to drugs for HIV and hepatitis, as well as to other medications. [21, 22] Under compulsory licensure, a government has the power to grant a license to local pharmaceutical producers, allowing them to use a patent without the patent holder’s permission. In countries without production capacity, they may import the drug from elsewhere. A compulsory license is typically issued when a government determines that a disease is of high priority locally and urgent access to treatment is necessary. Drug companies that refuse to negotiate an affordable price leave countries with little choice but to issue compulsory licenses to produce or import otherwise inaccessible medications.
Compulsory licensing has allowed many leading middle-income countries (such as Brazil and Thailand) to provide affordable medicines for HIV/AIDS under nationally funded programs. Activists can encourage their governments to use this mechanism if voluntary licensing (when the patent holder gives another party the right to manufacture, import, or distribute its pharmaceutical product) is not an option. Then governments can produce or import safe and effective PEG-IFN biosimilars.
Access to Biosimilars
A number of countries are using locally produced peginterferon (both biosimilar and alternative). These are available at a fraction of the cost of the originator products, allowing governments (such as Egypt’s) to treat large numbers of people. The availability of cheap PEG-IFN biosimilars has an impact on pricing: biosimilars and alternatives can be used as a leverage to negotiate cheaper prices with Roche and Merck.
The quality of internationally available biosimilar drugs and diagnostics must be assured if countries are to confidently scale up HCV treatment programs. Activists are demanding that the WHO immediately establish mechanisms for assessing the safety and efficacy of biologic medicines and diagnostic tests. Producers must prove that their products have been made using Good Manufacturing Process standards. A WHO prequalification process is also needed to facilitate access to safe and effective drugs and diagnostics.
Local manufacturers will increase global access to their product by improving data collection practices and transparency to regulators. In turn, the WHO, the European Medicines Agency (EMA), and the U.S. Food and Drug Administration (FDA) should create a clear and harmonized regulatory pathway for approval of biosimilars.
Diagnostics
The availability of affordable, effective point-of-care (POC) diagnostic and staging tools is essential to the scale-up of integrated hepatitis C screening, testing, treatment, care, and support programs in LMICs.
Simplified diagnostic tests such as dried blood spots from a single finger stick and noninvasive methods such as the use of routine blood tests to stage liver disease can be quickly administered and greatly increase access to treatment and care. These and other tools must be quality-assured to be useable. Donor agencies including the Global Fund to Fight AIDS, Tuberculosis and Malaria and UNITAID should support the development of simple, accurate, and affordable HCV diagnostics and disease-staging tools, since their cost and complexity are major barriers to treatment. The WHO should promote access to affordable POC diagnostics by facilitating their regulatory approval and prequalification.
Civil Society
Dozens of grassroots groups and regional networks across the world are demanding that their governments face up to the HCV crisis, and work together to respond. World Hepatitis Day (July 28) has provided a springboard for activists. In 2012, the Eurasian Harm Reduction Network marked World Hepatitis Day by presenting the WHO, Roche, and Merck with the Hepatitis C Treatment Waiting List, a petition calling for “affordable, high-quality hepatitis C treatment.” They demanded high-level leadership, and deplored the monopoly on PEG-IFN. The petition was circulated globally, and now has nearly 6,000 signatories. At the International AIDS Conference in 2012, just prior to World Hepatitis Day, global activists interrupted a Roche side meeting to deliver a plate of decomposing liver to the organizers. While activists stood at the front of the room holding a banner that said “HIV/HCV: Silence = Death,” International Treatment Preparedness Coalition—Russia staffer Denis Godlevskiy led a call to action for Roche to drop the price of Pegasys and “stop eating our liver.”
In Ukraine, India, Thailand, and around the world, many people living with HCV contracted it through injecting drug use. The WHO considers people who inject drugs a high-priority group for targeted HCV prevention and treatment. [23] Evidence shows that scaling up HCV treatment in PWID is highly cost-effective when provided together with core harm reduction services such as OST and needle and syringe programs. [24] Until the rights of people who use drugs are fully realized, hepatitis C prevention and treatment efforts have little chance of success.
Defusing the Bomb
The availability of generics and biosimilars can dramatically reduce prices. Significant price reductions for medications and diagnostics will allow governments to integrate hepatitis C programs into national budgets. The AIDS movement proved this crucial point: drugs originally priced at US$10,000 per year could be generically produced for a fraction of the cost, thus greatly expanding access. Today, millions of people are on first-line HIV medications that cost US$100 per year. In sub-Saharan Africa, where countries face decimating HIV epidemics, access has increased 100-fold as a result. [25]
Providing HCV treatment benefits both individuals and communities. Treating HCV can also help prevent new cases, and potentially lead to the eradication of HCV globally. [26] Highly effective peginterferon-sparing and peginterferon-free regimens on the horizon that require shorter treatment duration and have fewer toxicities will facilitate treatment rollout.
The World Health Organization must agree to support governments to provide consistently high-quality, affordable PEG-IFN. Governments, in turn, must partner with civil-society organizations to develop and fully fund national plans to address their HCV epidemic. Both the Global Fund (which already subsidizes government HCV-testing and treatment programs), and UNITAID (whose market influence strategies help reduce the price of drugs and diagnostics) can affect global public health and access barriers. Their strategic interventions will help to overcome political and economic challenges in HCV treatment scale-up.
Activists are demanding that more must be done to dismantle the “bomb.” The revolution in hepatitis C treatment is providing the tools to do this. But therapeutic advances will mean nothing without universal access to the new treatments, and programs to deliver them in a culturally competent way. The 194 member countries of the United Nations have agreed that the rights to health and life are to be enjoyed by all, equally, without discrimination. People living with and at risk for HCV and their activist allies must keep fighting for these rights to be realized. As American social reformer, abolitionist leader, and former slave Frederick Douglass said, “Power concedes nothing without a demand.”
Endnotes
- Degenhardt L, Mathers B, Vickerman P, Rhodes T, Latkin C, Hickman M. Prevention of HIV infection for people who inject drugs: why individual, structural, and combination approaches are needed. Lancet. 2010 Jul 24;376(9737):285–301. doi: 10.1016/S0140-6736(10)60742-8.
- Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013 Apr;57(4):1333–42. doi: 10.1002/hep.26141.
- Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006 Oct;45(4):529–38. Available from:
http://www.journal-of-hepatology.eu/article/S0168-8278(06)00297-2/abstract. (Accessed on 2013 May 9) - World Health Organization. Viral hepatitis resolution [Internet]. 2010 January 23 (cited 2013 May 7). Available from:
http://apps.who.int/gb/ebwha/pdf_files/EB126/B126_R16-en.pdf. - Centers for Disease Control and Prevention (CDC). Progress toward prevention and control of hepatitis C virus infection—Egypt, 2001–2012. MMWR Morb Mortal Wkly Rep. 2012 Jul 27;61(29):545–9. Available from:
http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6129a2.htm. (Accessed on 2013 May 7) - Strickland GT. Liver disease in Egypt: hepatitis C superseded schistosomiasis as a result of iatrogenic and biological factors. Hepatology. 2006 May;43(5):915–22. Review. doi: 10.1002/hep.21173.
- Struthers, A. From schistosomiasis to hepatitis C: the spread of HCV in Egypt. MJoTa. 2007(1);3:213. Available from:
http://mjota.org/images/SpreadofHCVEgypt.pdf. (Accessed on 2013 May 7) - Esmat G. Egypt’s national HCV treatment program: key tactics and lessons. Presented at: 48th Annual Meeting of the European Association for the Study of the Liver; 2013 April 24–28; Amsterdam, the Netherlands.
- Maek-A-Nantawat W, Avihingsanon A, Ohata PJ. Challenges in providing treatment and care for viral hepatitis among individuals co-infected with HIV in resource-limited settings. AIDS Res Treat. 2012;2012:948059. doi: 10.1155/2012/948059.
- Lavanchy D. Evolving epidemiology of hepatitis C virus. Clin Microbiol Infect. 2011 Feb;17(2):107–15. doi: 10.1111/j.1469-0691.2010.03432.x.
- Knox R. Novartis ruling reverberates past India’s borders [Internet]. 2013 April 2 (cited 2013 May 7). Available from:
http://www.npr.org/2013/04/02/175997129/novartis-ruling-reverberates-past-indias-borders. - Biotechnology Industry Organization. How do drugs and biologics differ? [Internet]. 2010 Nov 10 (cited 2013 May 7). Available from:
http://www.bio.org/articles/how-do-drugs-and-biologics-differ. - Shukla S. Citizen News Service. Patients overturn first ever product patent on medicine in India [Internet]. [cited 2013 May 7]. Available from:
http://www.citizen-news.org/2012/11/patients-overturn-first-ever-product.html. - India’s Novartis Decision. New York Times editorial [Internet]. 2013 April 4 (cited 2013 May 7). Available from:
http://www.nytimes.com/2013/04/05/opinion/the-supreme-court-in-india-clarifies-law-in-novartis-decision.html. (Accessed on 2013 May 7) - Bajaj V, Pollack A. India’s supreme court to hear dispute on drug patents. New York Times [Internet]. 2012 March 6 (cited 2013 May 7). Available from:
http://www.nytimes.com/2012/03/07/business/global/indias-supreme-court-to-hear-long-simmering-dispute-on-drug-patents.html?pagewanted=all&_r=0. - Ukranian Community Advisory Board [Internet]. Condemned to death came to the Cabinet of Ministers. 2013 April 29 (cited 2013 May 7). Available from:
http://www.ucab.org.ua/en/node/253. - Open Society Foundations. Global snapshot: HCV epidemiology and response (background document). MSF/TAG/OSF HCV Meeting; 2012 September 24–25; Paris, France.
- Bichoupan K, Martel-Laferriere V, Ng M, et al. Estimated costs of telaprevir-based triple therapy, including adverse event management at the Mount Sinai Medical Center, NY: $195,000 per SVR12 (Abstract 795). Poster presented at: 48th Annual Meeting of the European Association for the Study of the Liver; 2013 April 24–28; Amsterdam, the Netherlands.
- Kaplan K. Help support inclusion of pegylated interferon on the World Health Organization’s Essential Medicines List. TAGline [Internet]. 2013 Winter (2013 May 7). Available from:
http://www.treatmentactiongroup.org/tagline/2013/winter/help-support-inclusion-pegylated-interferon-who-essential-medicines. - World Health Organization. Medicines: essential medicines: fact sheet. Geneva: World Health Organization; 2010 June. Available from:
http://www.who.int/mediacentre/factsheets/fs325/en. (Accessed on 2013 May 7) - IHS. Indonesia issues compulsory licences against seven HIV, hepatitis drugs [Internet]. 2012 October 12 (cited 2013 May 7). Available from:
http://www.ihs.com/products/global-insight/industry-economic-report.aspx?id=1065972339. - Knowledge Ecology International. Examples of health-related compulsory licenses [Internet]. [cited 2013 May 7]. Available from:
http://www.cptech.org/ip/health/cl/recent-examples.html. - Nelson PK, Mathers BM, Cowie B, et al. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet. 2011 Aug 13;378(9791):571–83. doi: 10.1016/S0140-6736(11)61097-0.
- European AIDS Treatment Group [Internet]. New antiviral treatment could significantly reduce global burden of hepatitis C. 2013 May 6 (cited 2013 May 7). Available from:
http://www.eatg.org/news/168169/New_antiviral_treatment_could_significantly_reduce_global_burden_of_hepatitis_C. - UNAIDS (Press Release). HIV treatment now reaching more than 6 million people in sub-Saharan Africa [Internet]. 2012 July 6 (cited 2013 May 7). Available at:
http://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2012/july/20120706prafricatreatment. - Hagan LM, Schinazi RF. Best strategies for global HCV eradication. Liver Int. 2013 Feb;33 Suppl 1:68–79. doi:10.1111/liv.12063.

