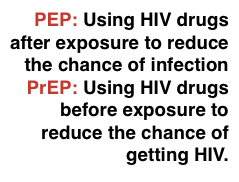
PEP and PEPSE?
PEP stands for Post Exposure Prophylaxis.
This involves using a combination of three HIV drugs after sex if there has been a significant risk – and taking them for a month. The word PEPSE is sometimes used – it stands for PEP after Sexual Exposure.
PEP needs to be taken as soon after exposure as possible. This is preferably within hours rather than days. Most guidelines have a cut off for PEP of 48 hours after exposure.
Even though in the UK you can get PEP for up to 72 hours it is much less likely to work when it is used this late. The longer the delay the less the chance that PEP will work.
Before getting PEP you will need to talk about your risk. This involves talking about the type of sex and whether you know the HIV status of your partner.
PEP is not prescribed in the UK unless there is a significant risk of HIV. For sexual exposure this generally needs to be sex without a condom when HIV status is unknown or if the partner does not have an undetectable viral load on ART.
For more details please see the UK (BHIVA) guidelines on PEP.
www.bhiva.org/PEP-guidelines (website link page)
www.bhiva.org/file/6183b6aa93a4e/PEP-guidelines.pdf (PDF)
You also need to have a rapid HIV test which gives the result within 30 minutes. This test only tells you whether you were HIV positive three months ago. It tells you nothing about the recent risk.
You need an HIV test because if you are HIV positive without knowing it, a short course of treatment could cause drug resistance.
You can get PEP at any accident and emergency (A&E) department of a hospital 24 hours a day. You can also access PEP from a GUM clinic during working hours.
After a course of PEP you need to wait 28 days before testing for HIV. This is because PEP can delay infection.
During the time on PEP, the meds might be keeping your viral load undetectable. However, even though HIV is difficult to catch, it is safer to use condoms until you know for certain whether or not you are HIV positive.
NOTE: If your partner was HIV positive and taking HIV treatment the risk to you may already be zero. It this case you don’t need PEP.
If an HIV positive has an undetectable viral load on treatment there is no risk of sexual transmission. This is also called U=U for undetectable = untransmissable. See U=U and below.
Can I use my partner’s meds as PEP?
Using someone else’s meds is not recommended. Some HIV drugs should never be used as PEP.
However, some HIV drugs have been studied for preventing HIV. These are tenofovir DF and FTC (in one pill called Truvada) and tenofovir alafenamide and FTC (in a single pill called Descovy). A single dose of either of these medicines would provide more rapid cover while you get to a clinic and wait to be seen.
TDF/FTC is now widely used to reduce the chance of HIV transmission when taken by HIV negative people. These studies also showed these drugs to be safe.
This would only be recommended as a single dose while you are waiting to get to HIV clinic for PEP.
However, if the HIV positive person is already on treatment and has an undetectable viral load, they will also be much less infectious. In these circumstances some guidelines think the risk is so low as to not recommend PEP.
In the UK, HIV meds that must NOT be used as PEP include:
- Any type of NNRTI (nevirapine, efavirenz, etravirine or rilpivirine).
- Atripla or Eviplera (which both contain an NNRTI)
- Abacavir (or Kivexa or Trizivir that contain abacavir).
This is because these drugs have a low risk very serious side effects, including hypersensitivity reactions and severe skin rash. With some NNRTIs the risk can be higher for someone with a stronger immune system that when they are used for treatment in someone who is HIV positive.
Some countries include efavirienz as part of PEP.
Last updated: 1 December 2022.