US Senate investigate Gilead for sofosbuvir price: potential to bankrupt Federal healthcare and add $300 annually to every American insurance premium for the next five years
1 August 2014. Related: Hepatitis coinfection.
 Simon Collins, HIV i-Base
Simon Collins, HIV i-Base
On 11 July 2014, the Committee of Finance of the US Senate – which has jurisdiction over social security funded health programmes (including Medicare and Medicaid) – wrote to Gilead Sciences CEO John Martin. The letter contained a comprehensive list of demands for disclosure of documents relating to the development, pricing and marketing costs for sofosbuvir, including all papers relating to Gilead’s acquisition of Pharmasset (who led early development of this drug) and is available online. [1]
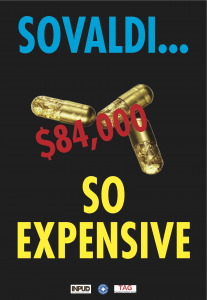
The investigation is into Gilead’s decision to charge $1000 for each sofosbuvir pill. A 12-week course of treatment costs $84,000 for the sofosbuvir component (additional meds are required) but for people requiring 24 or 48 weeks of treatment this increases to $168,000 and $336,000, respectively.
An estimated 3.2 million Americans are living with hepatitis C, more than half of who are incarcerated. Even if Medicare only treated 75,000 people in the next year, this would increase programme costs by $6.5 billion and increase premium costs for all enrollees by 8%.
Given such an impact on federal health programmes, the Committee is now investigating whether the price the Gilead set is “competitive, fair and transparent”. The letter raises this issue in the context of development costs for sofosbuvir at Pharmasset which for the three years from 2009-2011 was less than $180 million, with only $62 million directly attributed to sofosbuvir. It also notes the significant difference between the 44% discount offered to treat US prisoners with the 99% discount arranged with the Egyptian government.
The Committee also raises the “substantial risk of a conflict of interest” between individual panel members of the three main professional associations responsible for producing treatment guidelines – the American Association of the Study of Liver Disease (AASLD), the Infectious Diseases Society of America (ISDA) and the International Antiviral Society-USA (IAS-USA) – with 17 out of 27 members disclosing either direct or indirect financial relationship with Gilead.
The letter demands breakdowns of marketing costs and patient assistance programmes (through which, 30,000 people have received sofosbuvir in the US).
Gilead has 14 days to start producing information and 60 days to produce the complete dossier.
The price of sofosbuvir is also estimated to have a dramatic impact on private healthcare in the US.
In a letter to the Journal of American Medicine, CVS Caremark, one of the largest US pharmacies has estimated that the current price of sofosbuvir could add $200-$300 a year to every American insurance premium for the next five years. It also notes that universal treatment in the US alone would generate more than $250 billion for Gilead, and this would be inappropriately high at more than a 20-fold return on the acquisition cost of Pharmasset. [2]
Comment
The scope of this Senate committee investigation into corporate greed is interesting for several reasons. And this PR disaster for both Gilead and its shareholders is not going away.
Firstly, it reconnects drug pricing to the actual cost of development, including marketing – which in this case appears well under the $1 billion commonly quoted – and which has already been recouped many times over during the first months of licensing (Gilead earned over $3 billion in the first quarter of 2014). Gilead have so far tried to justify the price based on a model of potential lifetime savings compared to current treatment. [3]
The acquisition costs of $11 billion for a compound that had cost well under $200 million to develop, makes Pharmasset equally responsible for this low point in healthcare research.
Secondly, it raises issues of ethical pricing in the context of population need and the overall ability for any health system to be able to adequately provide treatment for the majority of people who need it. Gilead’s price, by definition, limits access to less than 1% of people with hepatitis C, even in rich countries. The investigation challenges the ethics of allowing a company absolute freedom in setting a price for a medicine.
Most shamefully, Gilead could easily have recouped the same level of profits by setting a significantly lower price – given the numbers of people needing treatment – and treating far more people. Setting a price that excludes more than 99% of people who could benefit from treatment is difficult to interpret as anything but greed.
Thirdly, it highlights the very low production costs that enable a 99% discount to Egypt to still be financially viable and profitable for the company. Independent analyses of manufacturing costs are estimated at less than $200 for a three-month course of treatment. [4] Importantly, this work has driven a community demand for total cost of HCV treatment to become US$500 or less for low- and middle-income countries. [5]
Whether this Senate committee has the resolve to change things or this is simply window-dressing in preparation for the next US elections, also remains to be seen.
In the UK, where more than 200,000 people are estimated to be living with hepatitis C, the price of sofosbuvir has forced the NHS to only commit to using it to treat 500 people with the most advanced liver disease. It also forced NICE to examine cost effectiveness for each combination of HCV genotype and stage of infection together with each permutation of prior HCV treatment history. [6]
References:
- US Senate Committee of Finance. Letter to John C Martin, Chair and CEO of Gilead Sciences. (11 July 2014).
http://www.finance.senate.gov/imo/media/doc/Wyden-Grassley%20Document%20Request%20to%20Gilead%207-11-141.pdf (PDF) - Brennan T, Shrank W. New expensive treatments for hepatitis C infection. JAMA. Published online July 20, 2014. doi:10.1001/jama.2014.8897.
http://jama.jamanetwork.com/article.aspx?articleid=1890401 - Collins S. Activists protest the price of sofosbuvir: “So-Valdi, So-Expensive” – UK access already rationed. HIV Treatment Bulletin, May 2014.
https://i-base.info/htb/25884 - Hill A et al. What is the minimum cost per person to cure HCV? 7th IAS Conference on HIV Pathogenesis, Treatment and Prevention, 30 June – 3 July 2013, Kuala Lumpur. Late breaker poster TULBPE16.
http://pag.ias2013.org/abstracts.aspx?aid=3142
http://pag.ias2013.org/EPosterHandler.axd?aid=3142 (Poster PDF) - Médicines sans Frontières Access to Medicines campaign. MSF responds to reports on Gilead pricing for hepatitis C drug sofosbuvir in developing. (03 February 2014).
http://www.msfaccess.org/content/msf-responds-reports-gilead-pricing-hepatitis-c-drug-sofosbuvir-developing-countries - NHS England. NHS England agrees funding for life-saving hepatitis C drug. (16 April 2014).
https://www.england.nhs.uk/2014/04/16/hepatitis-c/

