HIV in the UK 2014: Public Health England report on incidence and care
1 December 2014. Related: HIV prevention and transmission, Other news.
 Simon Collins, HIV i-Base
Simon Collins, HIV i-Base
The latest Public Health England (PHE) report on HIV in the UK was published on 17th November 2014, based on data collected to the end of 2013. [1]
The 50-page report has 15 appendices of summary data tables showing HIV incidence, patterns of infection and HIV management outcomes, including breakdowns by age, gender, risk group and geographic location. The report also includes data on other STIs and tuberculosis.
The following key findings are highlighted from data related to UK figures for 2013.
Selected overall results
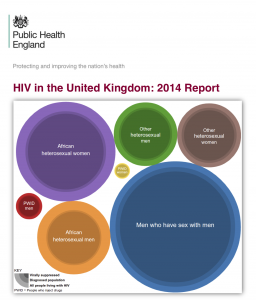
- 107,800 people are now estimated to be living with HIV in the UK (95% credible interval 101,600-115,800).
- Overall adult prevalence (aged 15-59 years) is now 2.8 per 1,000 population (1.9 per 1,000 women and 3.7 per 1,000 men).
- A quarter (24%, 26,100) of people living with HIV are not yet diagnosed. They risk HIV progression and ongoing transmission if they are not consistently using condoms.
- 6,000 people were diagnosed in 2013, and 98% were linked to care within three months.
- Of the 530 HIV positive people who died, 210 were younger than 60 years old. Late diagnosis is associated with a ten fold increase mortality risk in the first year after diagnosis, compared with diagnosis at a CD4 count >350, but this difference is driven almost completely by those diagnosed very late (CD4 <100).
- 42% (2,500/5,960) of people were diagnosed late, defined by having a CD4 count less than 350 within three months of their diagnosis. 62% of heterosexuals and 31% MSM were diagnosed late. The CD4 count was lower than 200, categorised as extremely immunocompromised, for 24% diagnosis (1,430).
- The report notes that people living with HIV can expect a near-normal life span if they are diagnosed while their CD4 count is still above 350. People diagnosed later have a ten-fold increased risk of death in the year following diagnosis compared to those diagnosed earlier.
- 81,500 people received HIV care in 2013 (55,200 men and 26,300 women). This is a 5% increase on the previous year (77,590) and almost double the number a decade ago (41,160).
- One in four people living with diagnosed HIV is now older than 50 years. This is mainly related to the impact of effective treatment that means we live longer. This shows the importance of developing services that are appropriate to an ageing population.
- Data on recent infections highlights that ongoing transmission is a risk at all ages.
Gay, bisexual and other MSM
- HIV still disproportionally affects gay, bisexual and other men who have sex with men. The number of MSM diagnoses was a record high (3250/6000). This approximates to an adult prevalence of 59 per 1,000. In London, an estimated 1 in 8 MSM are HIV positive compared to 1 in 26 outside London.
- By age, 16% of new diagnoses were in men younger than 24 and 10% were in men older than 50.
- Based on RITA data from 1080 MSM, approximately 30% indicated recent infection.
- Approximately 16% of MSM are undiagnosed (~7,200). This percentage has been consistent for the last ten years. Most of these people are likely to have been recently infected (in the last 1-2 years).
- 25% of newly diagnosed MSM had concurrent acute STIs (chlamydia, gonorrhoea and/or syphilis). This compared to 5.9% and 2.8% among newly diagnosed heterosexual men and women respectively.
- Using a back calculation analysis based on CD4 count at diagnosis, the report estimated that 2800 MSM were infected in 2013 – a number that has been broadly consistent annually for the last ten years.
Transgender people
- No data is presented for transgender people, despite disproportionally high rates reported in other countries. However, trangender data will now be collected through HARS, the new HIV surveillance system.
Heterosexual transmission
- Approximately 59,500 people in the UK are living with HIV due to heterosexual transmission.
- Based on RITA data from 657 samples, approximately 13% indicated recent infection.
- A steady decline in new heterosexual infections is related to fewer diagnoses in people born in sub-Sahara Africa. However, approximately 60% of infections occurred in the UK (1500/2490).
- HIV disproportionally affects black Africans (~65% of heterosexual infections).
- Adult HIV prevalence among black-African heterosexuals is 56 per 1,000 (71 per 1,000 women and 41 per 1,000 men). This compares to prevalence of 0.6 per 1,000 for non black-African heterosexual men and women.
- Approximately 31% of heterosexuals are undiagnosed (~18,500). This includes 13,000 black-Africans (almost two in five men and one in three women).
People who inject drugs (PWID)
- Infection through drug use remained low with 130 cases, similar to the previous two years.
Mother to child transmission
• 90 new diagnosis were related to mother to child transmission, with the vast majority of cases occurring outside the UK.
Treatment cascade
- 76% of people living with HIV are diagnosed.
- >98% of people diagnosed were seen in care (CD4 count within 3 months).
- >95% of people in care retained in care.
- 90% of adults seen for HIV care in 2013 were prescribed ART.
- 90% of all adults receiving ART were virally suppressed <200 copies/mL.
Comment
These figures clearly show that HIV is far from ended in the UK, with more than 500 people diagnosed each month.
Current prevention programmes are particularly failing young gay men with 16% of MSM diagnoses last year (460 people) in men aged less than 24 years. This highlights the urgency of an early access programme for the option to use PrEP for those at highest risk.
It is unclear why uptake of RITA testing is still so under-used, given that this is paid for centrally, but expanding this to clinics that currently do not use the service would improve our understanding of recent infections.
Of the 90 MTCT transmissions, two thirds were in adults – virtually all born abroad and arrived in UK as adults, but reported as newly diagnosed in 2013 in the UK, with MTCT as likely mode of acquisition. Even among the 34 under 16 year-olds newly diagnosed in 2013, few were UK born and all but 2 were born prior to 2012. The actual MTCT rate in the UK is around 0.5% for women diagnosed prior to delivery. [4]
Although there are currently still no data on HIV rates in transgender communities, recent discussions between tansgender activists and PHE indicates that sexual health clinics will now be expected to collect gender data in non- binary categories. Hopefully, the long-standing lack of data for how HIV affects trangender people, might allow first data to be included in the 2015 report.
The PHE report also includes the importance of new approaches to HIV prevention, including calling for a more rapid access to PrEP. Bringing HIV testing to those people currently unaware of their HIV status and routine testing for those at highest risk are clearly critical stages in the UK cascade. Without this, benefits from both TasP and PrEP are unlikely to dent the ongoing incidence.
2015 needs to be branded as “HIV testing year”. Opt-out HIV testing in sexual health clinics is one key recommendation in the report that could help. Having had a recent HIV test needs to become a social norm, especially across all the highest incidence communities.
The UK is fortunate to still have one of the most comprehensive and careful surveillance programmes: this report is essential for the breadth of data and analysis that it contains. However, a few relatively small points from this otherwise excellent service might be useful feedback for 2015.
Firstly, although the report includes page of “PHE messages” apparently aimed at a general reader, this is the least useful section. It is good to include a non-technical summary but this needs to be more appropriately considered. Advice to “avoid overlapping relationships” is unlikely to lead to significant behavioural change.
Secondly, the use of the term “unprotected sex” is outdated and needs to be replaced by language specifying when this means not using a condom, given the prevention benefits of TasP and PreP.
Thirdly, most pages on the PHE website look and feel more like the prison service or tax office. Even if the HPA has gone, a little colour, warmth and a few graphics would help – given that these cost nothing.
References:
- Public Health England. HIV in the United Kingdom: 2014 report. 18 November 2014.
https://www.gov.uk/government/statistics/hiv-in-the-united-kingdom - HIV data tables are available at:
https://www.gov.uk/government/statistics/hiv-data-tables - The 2014 HIV Surveillance Overview will include estimates of undiagnosed HIV infection, HIV incidence trends, the impact of treatment as prevention and the monitoring of HIV care quality.
http://www.phoutcomes.info/public-health-outcomes-framework#gid/1000043/pat/6/ati/102/page/0/par/E12000004/are/E06000015 - Townsend CL et al. Earlier initiation of ART and further decline in mother-to-child HIV transmission rates, 2000–2011. AIDS 2014, 28:1049–1057. DOI:10.1097/QAD.0000000000000212.
http://www.ncbi.nlm.nih.gov/pubmed?term=24566097

