High cure rates using generic hepatitis C drugs bought online: EASL supports lower cost access for Western countries
1 June 2016. Related: Conference reports, Treatment access, Hepatitis coinfection, Other news, EASL 51 Barcelona 2016.
 Simon Collins, HIV i-Base
Simon Collins, HIV i-Base
A new way to access excessively priced drugs in high-income countries, including the UK, was presented today in an oral late-breaker study at the 2016 International Liver Congress (EASL) currently being held in Barcelona.
Just as importantly, this approach to access treatment was officially supported by EASL.
James Freeman from GP2U Telehealth and colleagues presented interim results from an international cohort of people using generic HCV drugs bought online using a web-based community project in Australia (FixHepC.com). [2]
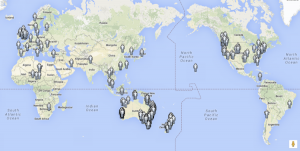
Countries with people enrolled into FixHepC.com programme.
The high prices charged for new HCV drugs has enraged many doctors, researchers and people living with HCV, who in good faith supported the drugs’ research and development, with the expectation that people in the countries where this was conducted would widely benefit.
Instead, the research showing extraordinarily high efficacy and safety – curing more than 95% of patients within a few months of easy-to-take treatment – led to drugs that, post-approval, remain out-of-reach, with access filtering through to only a few of the most sick or richest.
The unethical nature of this example of pharmaceutical pricing is highlighted by the production and manufacturing costs, which for all of these HCV medicines are incredibly low, together with the unmet medical need by 150 million HCV positive people globally. Last year, more people died from HCV-related complications than were treated with these medicines.
Another presentation at the conference on the cost of HCV drugs, by Andrew Hill from the Chelsea and Westminster Hospital in London, showed that the raw material for the combination of sofosbuvir plus declatasvir was less than $100 for a three month course of treatment but this is priced at US $84,000 in the US and about US $50,000 in the UK, France and Australia. [3]
As a result, even after being recently approved by NICE in the UK, only the sickest people will be treated, while everyone else waits for trickle-down access over years or decades.
But, it is legal in the UK, Australia and some other countries, for citizens to important generic medicines bought online, so long as this is for their personal use. Personal use is defined as being for three months or less. Many other countries allow generic medicines to be imported personally when carried by the individualwho is using treatment. This is included in the TRIPS agreement (article 60) in reference to patent agreements. A community web-based project in Australia (FixHepC.com) was set up to help facilitate this access.
FixHepC.com first validated the quality of generic sofosbuvir, ledipasvir, daclatasvir and ribavirin using high performance liquid chromatography (HPLC) and mass spectrometry. So far, 448 people have enrolled and been helped though the steps needed to import medicines. Clinical assessments were made before, during and after treatment using a telemedicine platform (gp2u.com.au).
This is an international cohort with people enrolling from the UK, Europe, Australia, the United States, Thailand, Africa and South America. Mean age was 54 and almost half were women (46%). Baseline genotype (G) was approximately 64% for G1, 5% G2, 27% G3, 3% G4 and <1% G5/6. Half the participants were treatment naive (51%) and almost one-third (31%) had cirrhosis. Mean HCV viral load was 6.46 log IU/mL.
Treatment results were available for about half of the cohort. End of treatment (EOT) and sustained viral response rates at week 4 (SVR4) were 99.6% (220/221) and 94.2% (129/137) respectively. SVR4 results were 94.2% (129/137) overall for G1-6. By regimen, G1 results were 93.2% (55/59) using sofosbuvir plus ledipasvir and 97.4% (37/38) for using sofosbuvir plus daclatasvir.
SVR4 results by genotype, recognising there are very low numbers in some groups, were 95% (92/97) for GI, 100% (6/6) for G2, 90% (26/29) for G3, 100% (3/3) for G4 and 100% (2/2) for G5/6.
Tolerability was good, with no new side effects and headache, fatigue and insomnia being most reported.
Three people with compensated liver disease temporarily decompensated after starting treatment but continued with treatment.
Four people died, all from hepatic cellular cancer (HCC), one before starting treatment, two people discontinued treatment for palliative care, and one died before reaching the SVR4 timepoint.
The study concluded that results using generic imported HCV drugs are at least as effective and seen in clinical trails and that mass global treatment is feasible and a legal alternative for many people when high prices prevent access to originator drugs.
An official conference press release quotes Professor Laurent Castera, EASL Secretary General in support of this study: “There is a clear role for generic treatments such as these for people with hepatitis C across the world. The implications of increased availability of these drugs could be enormous, presenting more people with the possibility of a ‘cure’ for what is often a debilitating condition.” [4]
Comment
These results are important for indicating that generic HCV drugs purchased online using the FixHepC web service produced cure rates that are comparable to those reported in clinical studies of originator drugs.
Even though limited data are available from this interim analysis of an open-label study, the results also highlight that people in high-income countries are dying from HCV-related complications due to limited access to new treatment.
Although in the UK, the NHS should provide these drugs, the lack of government action to negotiate appropriate prices for medicines and the constrained NHS budgets that cannot afford current prices, mean that people might have to buy their own medicine to guarantee short-term access. Under these circumstances, as with PrEP for HIV prevention, the NHS should at least provide the monitoring needed to use these treatments safely.
At some point the originator manufacturers will reduce prices because their business models allow much lower prices to still generate vast profits from HCV drugs.
But companies will only do this if they are forced to and unfortunately the UK has shown no leadership for this to happen so far.
The support from EASL for using online generic medicines to access treatment is significant. There is little point in international meetings showcasing clinical results, however impressive, when these medical advances are being undermined by prices that prevent doctors from prescribing these medicines.
Reference:
- Freeman J et al. High sustained virological response rates using generic direct antiviral treatment for Hepatitis C REDEMPTION-1. International Liver Congress (EASL) 13-18 April 2016, Barcelona. Late breaker oral abstract LB03.
- FixHepC website.
http://www.fixhepc.com - Hill A et al. Significant reductions in costs of generic production of sofosbuvir and daclatasvir for treatment of hepatitis C. EASL 2016. Abstract number to follow.
- EASL press release. Low-cost generic direct-acting antiviral treatment for hep C is equivalent to branded formulations: New data indicate that generics are a feasible alternative to support access to direct-acting antiviral treatment for hepatitis C sufferers. 16 April 2016.
http://www.eurekalert.org/pub_releases/2016-04/eaft-lgd040816.php#.VxH_PRMb3Io

