HIV swine flu triage tools and flowcharts
23 August 2009. Related: Special reports, Other news.
HIV swine flu telephone triage tool
The following resource was developed by Birmingham Heartlands Hospital and is to be used with flow diagram HIV and Influenza H1N1v. This is an empirical protocol drawn up by individuals with some experience in the recent UK swine flu outbreak. Modifications have been made following a meeting at the HIV/ IAS conference 2009 in July. This is just one suggested clinical approach.
Please use and adapt this to your own clinic, if you would like to suggest improvements or share experiences please contact:
steve.taylor@heartofengland.nhs.uk
As they are produced, updated drafts will be posted online:
http://www.sexualhealthbirmingham.co.uk
Inquiry re HIV and swine flu: a suggested approach
- Does the patient have symptoms consistent with typical flu?
FLU DIAGNOSTIC CRITERIA
- An acute-onset illness with history of feeling feverish and confirmed temperature >38°C
- AND flu-like illness (two or more of the following symptoms: cough, sore throat, runny nose, limb/joint pain, headache)
- Significant diarrhea has also been described by several clinicians
If they fulfil the above criteria but have none of the conditions * or symptoms ** listed below, then advise the patient that they may be suffering from flu. Treatment can be obtained by calling the pandemic flu service line on 0800 1513 100 / 0800 1513 200 or visiting the website:
http://www.direct.gov.uk/pandemicflu
- They should be advised NOT to attend hospital unless they deteriorate, or if symptoms fail to improve within 48 hours of commencing flu antivirals, when they should be clinically assessed.
- Reassure them that its appears safe to take antiretrovirals (ART) with flu antivirals e.g. oseltamivir (Tamiflu).
- Although there is the potential for drug interactions between ART and osteltamivir we have taken the approach that potential benefits exceed the potential for side effects. Obviously this can be modified as new data emerges.
- The theoretical interactions with renally excreted drugs and osteltamivir have led us to recommend that if patients have significant renal impairment (ie eGFR <40 mL/min) inhaled Zanamivir can be considered as an alternative (see below).
- In pregnancy we have recommended inhaled Zanamivir (Relenza). However systemic treatment should not be withheld if the clinical condition warrants treatment. (Deaths have occurred in pregnant women who maybe at greater risk of severe infection).
- Reassure the patient that most people with uncomplicated flu will be significantly better within 48hours.
- Alternatively persons with severe symptoms that are not classically flu-like should be assessed and have flu swabs performed since a negative test can be very informative.
If the patient meets the flu diagnostic criteria above ANDhas any of the following conditions* then they need to be assessed by the ID/HIV/GU registrar on call for the day ______________________________ : [INSERT APPROPRIATE NUMBER]
- Conditions requiring assessment by a registrar:
- Pregnancy (any trimester)
- Asthma and other chronic lung disease
- Morbid obesity
- Significant immune suppression
Note: We suggest assessing patients with CD4 counts <200 or CD4% <15% with symptoms as they may have an alternative non-flu diagnosis. These cases should be discussed with a senior member of the HIV team or the ID /HIV/GUM registrar on call.
If the patient meets the flu diagnostic criteria above, but also has any of the following symptoms** they should be assessed by the ID/HIV/GUM registrar on call for the day immediately.
** Additional symptoms requiring immediate assessment
- Significant breathlessness or patient is unable to complete sentences
- Hypoxia <94% on air
- Unable to tolerate oral fluids or has significant vomiting
- Confusion
- Hypotension systolic BP <90
- If the patient has already received flu antivirals and is not showing signs of improvement after 48 hours or is feeling worse.
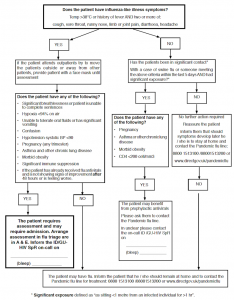
Flow diagram A: HIV and Influenza H1N1v (Birminham Heartlands Hospital)
HIV patients may come into contact with hospital services in various ways. Flow diagram A outlines a suggested protocol for 2 of a common scenarios: telephone contact to members of the HIV team or unplanned presentation to HIV/ID/GUM outpatient clinics.
Treatment
- Flu antivirals should be obtained by the patients calling the pandemic flu service line on 0800 1513 100 / 0800 1513 200 or visiting the website: http:www/direct.gov.uk/pandemicflu
- Oseltamivir (Tamiflu) is the currently recommended first-line flu antiviral for most HIV patients and it should be commenced immediately. The dose is 75 mg bd for 5 days.
- In patients with significant renal impairment (eGFR <40 ml/min) or pregnant women we would consider using inhaled zanamivir (Relenza) as an alternative. However, If symptoms are significant, discussion should be sought with senior member of the HIV team with regards to the use of osteltamivir.
- Inhaled zanamivir: Two 5mg blisters are to be inhaled (using the Diskhaler) twice a day for at least five days (equivalent to 10mg twice a day for five days). The patient needs to be capable of using disk haler for administration.
- If intolerant of zanamivir, oseltamivir may be used with caution +/- dose modification. For further information contact ID/ HIV/GU registrar on call [INSERT NUMBER AND BLEEP].
Prophylactic/post exposure treatment
- For HIV positive patients with CD4 > 200 or >15% we would not routinely recommend prophylaxis but instead suggest standard treatment IF the patients develops symptoms and meets the flu criteria above.
- For HIV positive patients with CD4 <200 or <14% prophylaxis may be considered in cases of significant exposure. However to date there is no data to suggest that these individuals are at increased risk of severe disease.
- Please remember in patients with CD4 counts <200 or <14% other opportunistic infections may present with flu like symptoms and patients should have diagnostic swabs to aid diagnosis and be discussed with a senior HIV doctor or ID/HIV/GUM SPR on call.
- For a usable definition we have classified significant exposure as sitting <1 metre from an infected individual for >1 hr.
- The oseltamivir (Tamiflu) dose when used as prophylaxisis 75 mg od for 10 days.
- Inhaled zanamivir: Two 5mg blisters are to be inhaled (using the Diskhaler) once a day for at least ten days (equivalent to 10mg twice a day for five days) The patient needs to be capable of using diskhaler administration.
Diagnostic swabs for influenza
- Although swabbing is now not routinely being performed we would advocate taking swabs in individuals infected with HIV as knowledge of negative results may be useful. The patient does not have to attend hospital for this and can be organised via GP or flu treatment centres.
Flow diagram B (Chelsea and Westminster Hospital, London)
The second example flow diagram was produced for managing patients at the Chelsea and Westminster Hospital in London.
A caution with this option is that a patient with a life-threatening condition who thought they had flu could end up going down the left-hand no further action route. The standard government advice on risk factors (eg. chronic heart, renal, liver, neurological disease), is non-evidence-based and may not be relevant in this (or possibly any) flu outbreak. It also does not address exposure
Does the patient have influenza-like illness symptoms?
- Temp >38°C or history of fever AND two or more of:
- cough, sore throat, runny nose, limb or joint pain, diarrhoea, headache
NO ? Assess the patients symptoms and triage as you would for any other patient telephone enquiry.
YES ? Do they have any of the following underlying conditions?
- Advanced HIV disease with CD4 <200 (or <14%)
- Pregnancy
- Asthma
- Chronic lung disease, chronic heart disease, chronic renal disease, chronic liver disease or chronic neurological disease
- Malignancy currently being treated, or having been recently treated with chemotherapy
- Other immunosuppressing conditions
- Any condition for which the patient is receiving immunosuppressing medication
NO ? Do they have any of the following symptoms?
- Significant breathlessness or are unable to complete sentences
- Increased rate of breathing
- Unable to tolerate oral fluids of has significant vomiting
- Confusion, striking agitations, visual disturbance, limb weakness or seizures
- Irregular heart beat/palpitations or chest pain
- Blood-stained sputum
NO ? Advise the patient that they may be suffering from flu and that they need to call their GP or the National Pandemic Flu Service on 0800 1 513 513 for further assessment. They should be advised not to attend hospital unless they deteriorate or there is no improvement.
YES ? Must be seen IMMEDIATELY in their nearest A&E
YES ? Do they have any of the following symptoms?
- Significant breathlessness or are unable to complete sentences
- Increased rate of breathing
- Unable to tolerate oral fluids of has significant vomiting
- Confusion, striking agitations, visual disturbance, limb weakness or seizures
- Irregular heart beat/palpitations or chest pain
- Blood-stained sputum
NO ? Must be assessed in Daycare or A&E if out of hours.
YES ? Must be seen IMMEDIATELY in their nearest A&E