WHO endorses “zero” transmission risk for people with HIV with an undetectable viral load
1 August 2023. Related: Conference reports, Treatment strategies, HIV prevention and transmission, IAS 2023 Brisbane.
Polly Clayden, HIV i-Base
 World Health Organisation (WHO) states that people living with HIV who have an undetectable viral load, using any WHO-prequalified test and sample, who are taking ART as prescribed, have zero risk of transmitting HIV to their sexual partner(s). And, people with a viral load that is suppressed to less than 1000 copies/mL, but that is still detectable, have almost zero or negligible risk of transmitting HIV to their partner(s), so long as they are still taking ART as prescribed.
World Health Organisation (WHO) states that people living with HIV who have an undetectable viral load, using any WHO-prequalified test and sample, who are taking ART as prescribed, have zero risk of transmitting HIV to their sexual partner(s). And, people with a viral load that is suppressed to less than 1000 copies/mL, but that is still detectable, have almost zero or negligible risk of transmitting HIV to their partner(s), so long as they are still taking ART as prescribed.
These announcements were made at the launch of a new WHO policy brief at a satellite symposium in the run up to IAS 2023. [1, 2]
The policy brief is supported by a systematic review published simultaneously in The Lancet, 23 July 2023. [3]
WHO policy brief: key messages
The brief is intended for a wide audience and is written in simple language.
It stresses that viral suppression is critical to improve health, prevent sexual transmission and reduce vertical transmission.
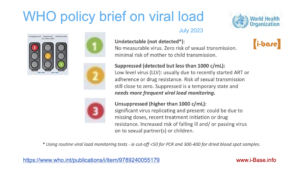
Viral load measurements are divided into three categories: (i) undetectable, (ii) suppressed, and (iii) unsuppressed.
These are illustrated by a traffic light system and defined as:
- Undetectable (not detected): no measurable virus. Zero risk of transmission to sexual partner(s); minimal risk of vertical transmission. Coded as green (for go).
- Suppressed (detected but less than 1000 copies/mL): some virus replicating and present. This could be due to recently starting treatment, intermittent adherence, or drug resistance. Almost zero or negligible risk of transmission to sexual partner(s). This situation requires three-monthly viral load monitoring. Coded as amber (for caution or get ready).
- Unsuppressed (greater than 1000 copies/mL): significant virus replicating and present. This could be due to missing doses, recently starting treatment or drug resistance. Increased risk of falling ill and/ or passing virus on to sexual partner(s) or children. Coded as red (for stop).
Any current WHO-prequalified tests and samples – including point-of-care tests and dried blood spot (DBS) samples – can be used to measure and define viral load results in the three categories. The sensitivity threshold for DBS is usually 300 – 400 copies/mL.
The brief also states that anyone with a detectable viral load – including suppressed to less than 1000 copies/mL should be supported with adherence counselling and a follow up viral load test.
And, “The ultimate goal for all people living with HIV is to reach and sustain undetectable viral loads. Taking ART as prescribed will support this goal, prevent transmission to their sexual partner(s) and/or children, and improve their own clinical well-being.”
Systematic review
>WHO conducted a systematic review to understand the clinical impact of being suppressed but detectable (less than 1000 copies/mL) and inform these new recommendations. This has important implications, particularly in low- and middle-income countries that use alternatives to plasma-based viral load testing.
The authors noted: “Although it is generally accepted that HIV viral loads of less than 200 copies/mL are associated with zero risk of sexual transmission and this threshold is used for U=U messaging in many high-income settings, the risk at virus levels higher than 200 copies per mL has been controversial.”
Studies included in the review looked at sexual transmission between serodifferent couples at various levels of viraemia (ie the evidence behind U=U), and the public health impact of low-level viraemia.
The authors identified 244 studies that might be relevant but only eight were included eight in the analysis, with 7762 serodifferent couples across 25 countries.
Three studies showed no HIV transmission when the partner living with HIV had a viral load less than 200 copies/mL. In the remaining four prospective studies, there were 323 transmissions – none were in participants considered suppressed on ART. There were two cases of transmission when the partner with HIV’s most recent viral load was less than 1000 copies per mL. But the authors noted that the interpretation of both cases was complicated by long intervals (50 days and 53 days) between the transmission date and the most recent viral load result.
The systematic review found no evidence of HIV transmission to sexual partners when viral loads were less than 600 copies/mL and an incredibly rare occurrence of possible transmissions with viral loads between 600 and 1000 copies/mL.
Importantly, the prevalence of low-level viraemia remains relatively low: one study found that among people with a suppressed viral load (less than1000 copies/mL), the majority (95%) had an undetectable viral load.
This suggests that the U=U message also applies to people living with HIV experiencing low-level viraemia.
The authors emphasised two important caveats to the results and in turn messages informed by the review.
First, that they do not apply to vertical transmission that can happen during pregnancy (ie in utero), at delivery or through breastfeeding, so the length and strength of exposure to viraemia is considerably more than that of sexual transmission.
Second that there are no data on risk of transmission through sharing of injection drug use equipment at varying levels of viraemia.
And, the authors noted that these outcomes have not been thoroughly studied in the context of current, optimal integrase inhibitor-based ART.
They also note that people with suppressed viral load need more frequent viral load monitoring – ideally every three months – to determine whether viral load is likely to be a temporary blip or genuine rebound.
They concluded: “An undetectable viral load should be the ultimate goal for clinical management of all people living with HIV on ART. However, the evidence showing almost zero risk of sexual transmission when HIV viral loads are less than 1000 copies/mL provides a powerful opportunity to destigmatise people who are living with HIV and promote adherence to ART through dissemination of this positive public health message.”
Testing and sampling
The policy brief also summarises the various WHO-prequalified viral load testing options available for national programmes to consider. [1]
These range from high-throughput laboratory based technologies to simpler point of care tests that can be decentralised.
Although considered to be the gold standard, collecting and processing plasma samples is too complex (storage, transport, laboratory equipment etc) in many settings and using alternatives, such as dried blood spots, can massively expand access to viral load testing.
Lower limits of detection of some tests and sample types tend to be higher than plasma (due to the smaller volume of samples) but this does not stop the technologies from correctly classifying people living with HIV as unsuppressed, suppressed or undetectable.
The brief includes a useful summary for programmes and healthworkers, describing typical viral load technology reporting outputs.
And it emphasises that all HIV viral load tests and sample types available and with WHO prequalification can accurately identify people living with HIV in the three viral load categories.
comment
That the generally measured-in-its-language WHO describes people living with HIV with an undetectable viral load by any WHO-prequalified test and take their ART as prescribed having “zero risk” of transmitting HIV to their sexual partner(s) is a big step forward.
It is also extremely useful to have clarification on the “almost zero or negligible risk” for people in the grey area below 1000 copies/mL. And notable that only 5% of these people are not also likely to be undetectable too.
The brief explains that suppressed below 1000 copies/mL is a transitory state – either in people who have just recently started ART or those whose viral load might be increasing. It is important that people in this situation are supported with adherence counselling and more frequent follow up viral load tests, ideally every three months.
The IAS listed this as one of its “Eight takeaways from IAS 2023” [4] And wrote: “This is a massive boost to the undetectable equals untransmittable (U=U) messaging.”
Overall this message is hugely important for people living with HIV in low- and middle-income countries who can now have the peace of mind about onward transmission in the same way that people in high-income countries do.
For national programmes and healthworkers it is also a critical message that all WHO prequalified viral load technologies can identify people living with HIV as unsuppressed, suppressed and undetectable. Dried blood spots particularly will help national programmes to ensure more widespread and equitable access to viral load for all people living with HIV.
References
- World Health Organization. The role of HIV viral suppression in improving individual health and reducing transmission. Policy brief. 22 July 2023.
https://www.who.int/publications/i/item/9789240055179 - What’s new in WHO guidelines: innovations, treatment, integration and monitoring. IAS 2023. Brisbane, Australia. 23–26 July 2023. Satellite session SAT026.
https://conference.ias2023.org/programme-live-1?coday=2023-07-23&embed= (session) – requires sign-in
https://conference.ias2023.org/media-1149-what39s-new-in-who-guidelines-innovations-treatment-integration-and-monitoring (abstract) – requires sign-in - Broyles LN et al. The risk of sexual transmission of HIV in individuals with low-level HIV viraemia: a systematic review. The Lancet. 23 July 2023.
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)00877-2/fulltext - Eight takeaways from IAS 2023.
https://www.iasociety.org/conferences/ias2023/takeaways-from-ias-2023