Taking a break from monkeypox: four weeks out for August
3 August 2022. Related: Special reports, mpox.
An option for individual and community health and to help our sexual health clinics.
Simon Collins, HIV i-Base
 The latest research into monkeypox (MPX) covered in this issue of HTB includes new information suggesting greater concerns about transmission during asymptomatic infections.
The latest research into monkeypox (MPX) covered in this issue of HTB includes new information suggesting greater concerns about transmission during asymptomatic infections.
Another study reports viral persistence of this particularly sticky virus on hard surfaces (washrooms, door handles, soap dispensers).
Language about the crisis has also changed. Instead of continuing to say that the primary goal is to prevent MPX from becoming endemic in new countries, some health experts now say this has already happenef and will continue to be so for at least the next few months. Some now say MPX is now endemic in gay, bisexual and other men who have sex with men.
This last suggestion is usually balanced by noting that viruses rarely follow social boundaries.
Public health messaging
Public health information is still largely focused on what to do if you might have been at risk from MPX:
- Be aware of symptoms (from fatigue, to rash, to ulcers).
- Self-isolate.
- Call a sexual health clinic or 111.
Public policy responses have also worked to reduce the risk of stigma and discrimination. Thanks to this strategy, mainstream media report MPX as an infection that anyone can catch.
Reducing risk
Just as many people are already reducing their risk, there is a role for direct information about the easiest way to avoid MPX.
- Talk to friends and partners about MPX.
- Exchange contact details with new partners – not a bad idea at any time.
- The best way to avoid MPX is to stop going to settings where it is easy to have contact with multiple partners – whether or not you have sex. MPX is very infectious.
This includes private parties, saunas, outdoor cruising areas, darkrooms and other sex-on-premises venues.
This information is to inform individual choice.
- It will be easier for some people and very difficult for others.
- But enough people doing this could also put a break in the outbreak.
- It will also support sexual health clinics who are first responders, so far with no additional funding.
Taking time for the vaccines to work
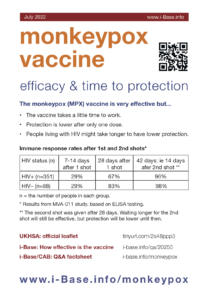
The MVA monkeypox vaccine is likely to be very effective but also takes a little time to work.
Efficacy data are currently limited to measuring immune responses in several studies, rather than reporting direction reductions in infections or symptoms. Some of these suggest that waiting up to four weeks might be important for highest levels of protection. This is also included in advice from the UKHSA. [1, 2, 3, 4]
Two of these studies suggest that four weeks might be especially important for people living with HIV. These studies are included in the EU SPC/EPAR and in the US evaluation that lead to vaccine approval. [5, 6]
Currently, very limited information about efficacy and time to protection is being given to people getting the vaccine. If people return to their regular lives before optimum vaccine cover, this could add to the current outbreak.
Many people are already reducing their risk especially if they are waiting for access to a vaccine. Awareness of MPX has steadily increased and it can range from mild but needing to self-isolate for three weeks, to painful and unpleasant, with possible scarring.
Severe infections have involved admission to intensive care units and a few cases have been fatal.
References
- UKHSA. Protecting you from monkeypox – information on the smallpox vaccination. (8 July 2022). [Updated 1 August 2022]
https://www.gov.uk/government/publications/monkeypox-vaccination-resources/protecting-you-from-monkeypox-information-on-the-smallpox-vaccination - Pittman PR et al. Phase 3 efficacy trial of modified vaccinia ankara as a vaccine against smallpox. N Engl J Med 2019; 381:1897-1908. DOI: 10.1056/NEJMoa1817307
https://www.nejm.org/doi/full/10.1056/NEJMoa1817307 - Overton ET et al. Safety and immunogenicity of modified vaccinia ankara-Bavarian Nordic smallpox vaccine in vaccinia-naive and experienced HIV-positive individuals: an open-label, controlled clinical phase 2 trial. Open Forum Infect Dis. 2015 May 5;2(2):ofv040. doi: 10.1093/ofid/ofv040.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4567089 - Greenberg RN et al. Safety, immunogenicity, and surrogate markers of clinical efficacy for modified vaccinia Ankara as a smallpox vaccine in HIV-infected subjects. J Infect Dis. 2013 Mar 1;207(5):749-58. doi: 10.1093/infdis/jis753. Epub 2012 Dec 7.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3611764 - EMA. Full prescribing information for Imvanex vaccine. (22 July 2022).
https://www.ema.europa.eu/en/medicines/human/EPAR/imvanex (webpage link)
https://www.ema.europa.eu/en/documents/product-information/imvanex-epar-product-information_en.pdf (direct PDF link) - US Office of Vaccines Research and Review (OVRR). Review memorandum for Jynneos vaccine. (2018)
https://www.fda.gov/media/131870/download (direct download) - i-Base Q&A. How good is the monkeypox vaccine?
https://i-base.info/qa/20255